LIVINGLIVING
An update on the encapsulation of precious insulin cells
funded by JDRF to treat Type 1 diabetes. By Rebecca Leitch,
who works at JDRF UK.
Encapsulation explained
As part of our research to find the cure
for Type 1 diabetes, JDRF is working to
develop techniques that will one day allow
people to regain insulin-producing beta
cells. In Type 1 diabetes, the beta cells
are killed off by the immune system, so
a technique called encapsulation is being
used to transplant new beta cells while
protecting them from another immune
attack. It is hoped that safely replacing the
lost beta cells for people living with T1D
will allow for the detection of changes in
blood glucose levels and the production
of insulin on demand - known as a
functional cure.
One encapsulation technique involves
protecting the transplanted beta cells
with a coating (alginate) that the immune
system doesn't respond to. Last August,
researchers in the US, partly funded by
JDRF, found an alginate in seaweed which
was able to coat and protect insulinproducing
beta cells for four months after
transplantation into monkeys, without the
need for immunosuppressant drugs. In
2016, JDRF supported the development
of a technique which involved weaving a
web of different molecules around sets of
islets (groups of beta cells) to create an
ultra-fine coating to protect them from
immune cells.
Another technique JDRF is supporting
is the development of a device that can
be implanted into the abdomen. This
product, developed by US company
ViaCyte, holds the cells safely inside the
device, which acts as a protective bubble
to keep them safe from immune attack.
Called the Encaptra system, it has holes
which are small enough to allow nutrients
through to enable the cells to live and
work, but won't let immune cells in.
Following the clinical trial at the
University of California, researchers found
that implanted cells survived and matured
into cells capable of producing hormones
including insulin and glucagon, but the
process of putting it inside the body
(engraftment) needs to be refined and
improved upon.
New options
There also is a newer encapsulation
product that is showing promising results
in this area. A firm has developed livecell encapsulation technology using
cellulose, a naturally-occurring plant
source that is free from impurities which
has been shown to last two years in the
body without breaking down or causing
damage to tissue nearby. The company
is working on encapsulating a human cell
line that has been designed to function as
a 'bio-artificial' pancreas when implanted
in a patient with Type 1 diabetes.
Finally, a team studying the protein
CXCL12 found it has a repellent effect on
immune cells and are using the protein to
drive immune cells away from the beta
cells they mistakenly try to attack in Type
1 diabetes.
Islet encapsulation has huge potential
to transform the lives of people with
Type 1 diabetes by eliminating daily
management of the condition. JDRF is
proud of the encapsulation projects that
we are supporting and is excited about
the potential of all the research happening
in this field, around the world.
www.jdrf.org.uk
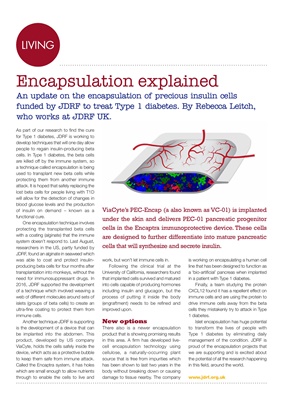
ViaCyte's PEC-Encap (a also known as VC-01) is implanted
under the skin and delivers PEC-01 pancreatic progenitor
cells in the Encaptra immunoprotective device. These cells
are designed to further differentiate into mature pancreatic
cells that will synthesize and secrete insulin.